Trigeminal neuralgia is a common neurologic disorder in which there are severe zaps of pain in the face. Patients often describe the pain as aching or stabbing or sometimes like an electric shock. The pain attacks start and stop suddenly, and they are brought on by everyday activities like brushing teeth, talking, chewing, or even a light breeze blowing across your face.
Trigeminal neuralgia is described as one of the most painful conditions known to man. The good news is that we have effective medicines like carbamazepine (Tegretol) and oxcarbazepine (Trileptal), as well as a variety of surgical options for patients who do not find relief with medications.
The most common cause of trigeminal neuralgia is irritation of the trigeminal nerve – a nerve in the head that supplies sensation for the face. In some people, this nerve is in contact with a blood vessel near the brainstem. With each beat of the heart, the blood vessel pulsates and bangs into the nerve. This eventually injures the nerve, and the nerve starts misbehaving, interpreting normal sensations as painful ones. Trigeminal neuralgia can also be caused by other disorders such as multiple sclerosis, stroke, and tumors inside the skull.
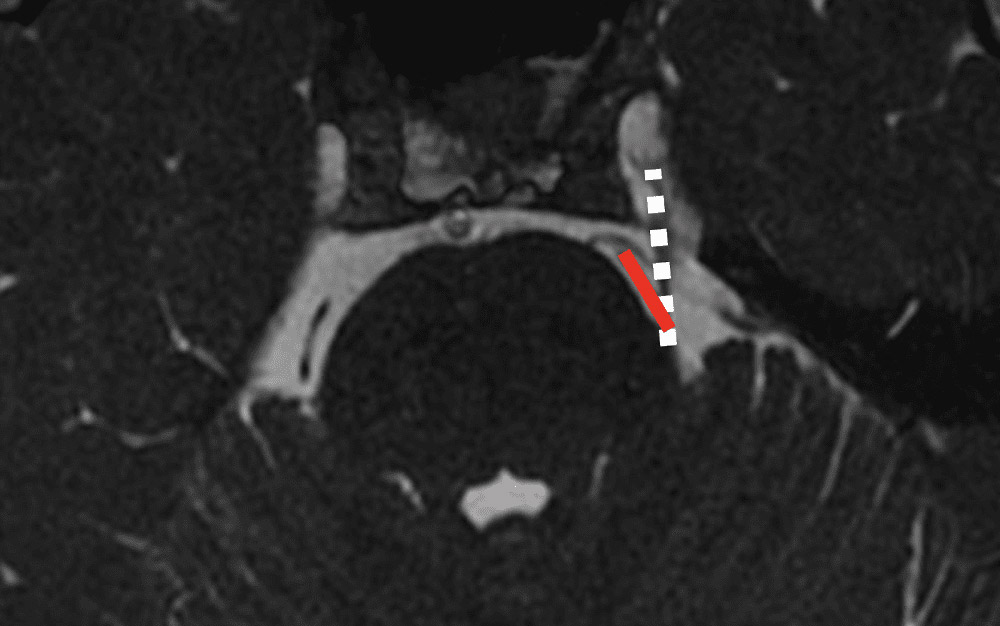
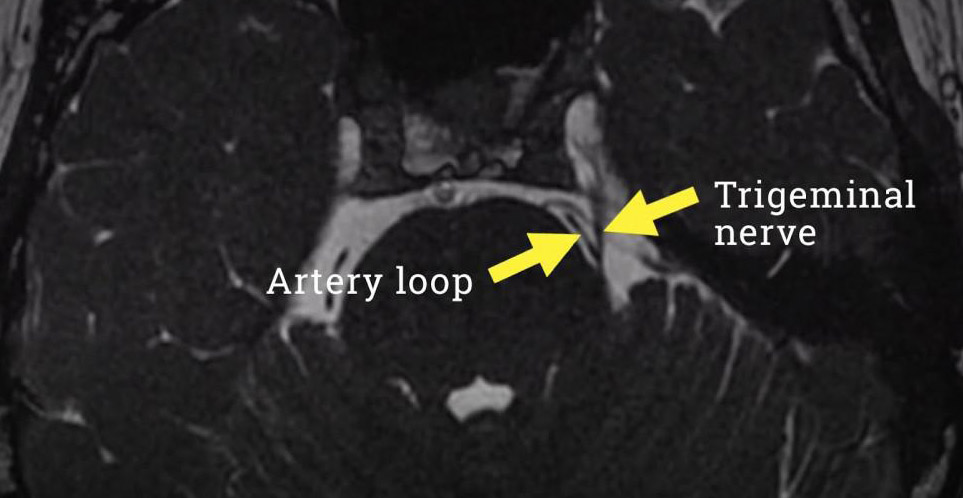
This is an example image from an MRI scan of the trigeminal nerve emerging from the brainstem. This dashed white is the trigeminal nerve, and the red line is an artery that is contacting the nerve. Each time this artery pulsates with the heartbeat, it bangs into the trigeminal nerve.
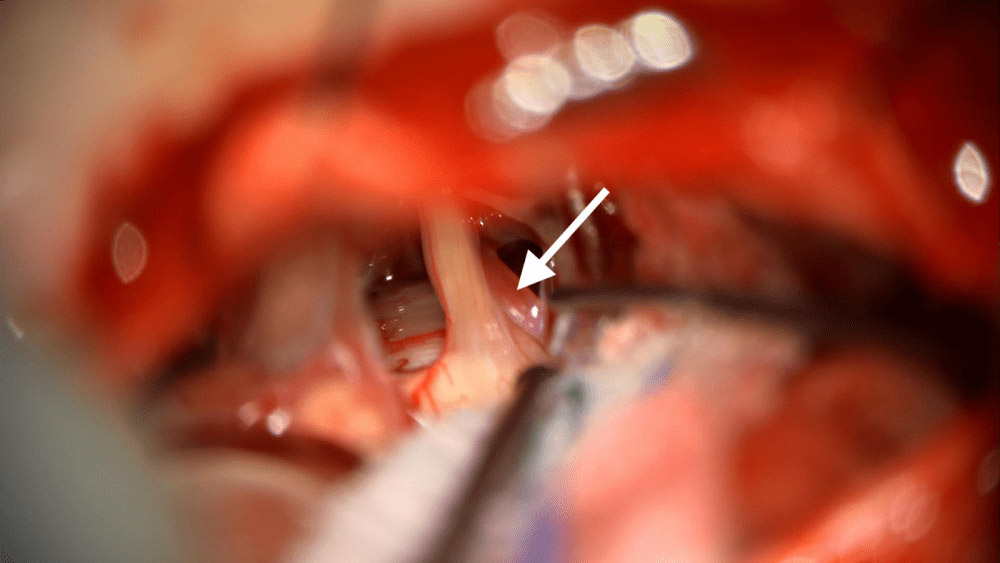
Below is a photograph from a procedure called a microvascular decompression. This is what the artery and nerve from the MRI look like in real life.The photo shows the trigeminal nerve and a nearby artery (white arrow) that is compressing it.
Trigeminal neuralgia and other forms of facial pain can be debilitating and life-changing. Many patients have seen dentists or oral surgeons, ENT doctors, neurologists, and other specialists before the problem is identified. My message to patients is there is hope. There are a number of effective therapies for facial pain, and some of them are relatively non-invasive. There is no need to suffer; I am committed to diagnosing and understanding your problem and creating a treatment plan that works for you.
Microvascular Decompression (MVD) for trigeminal neuralgia:
An MVD is perhaps the most effective and long-lasting surgery that we have for trigeminal neuralgia. It’s non-destructive, meaning that we don’t damage the nerve in the procedure (unlike other procedures for trigeminal neuralgia). As a result, there’s a comparatively low rate of facial numbness.
An MVD involves creating a small craniotomy behind the ear that I use to dissect down to the brainstem to access the trigeminal nerve.
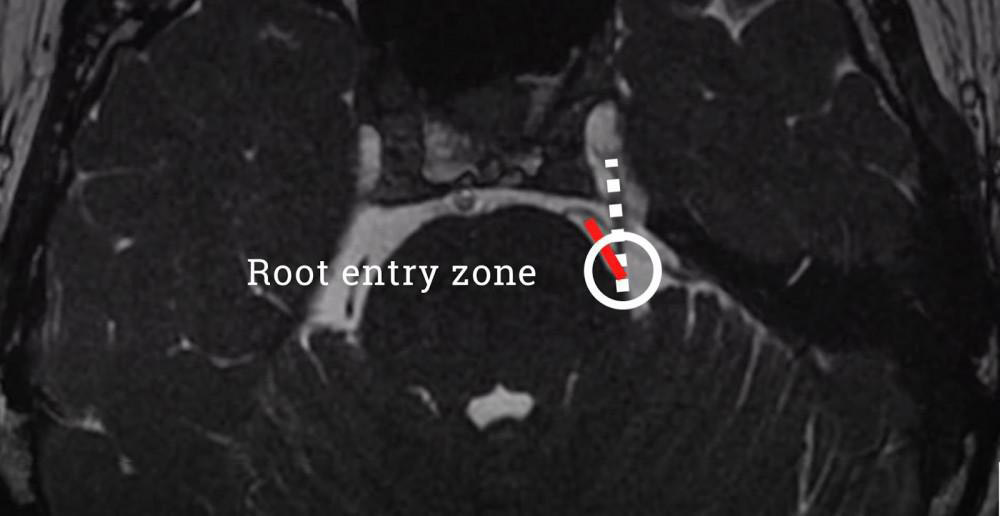
This is an MRI scan from a patient I treated recently with an MVD. In this MRI snapshot, you can see both the trigeminal nerve and a nearby loop of an artery that is coming in close contact with the nerve in a region of the nerve called the root entry zone. We know this part of the nerve is sensitive and irritable and that any compression of the nerve here can give rise to symptoms of trigeminal neuralgia.
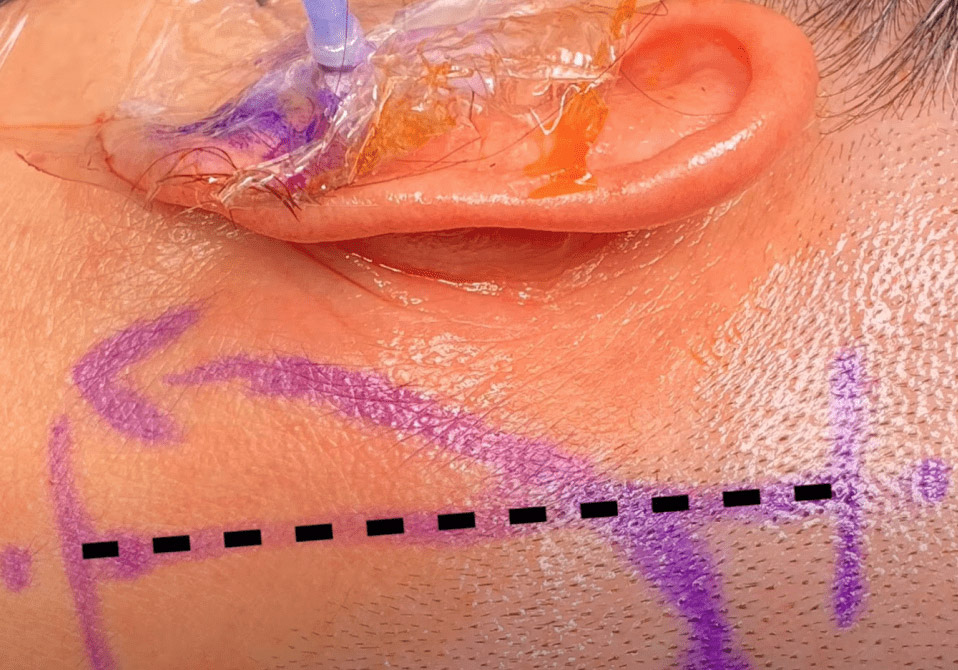
During surgery, I create a small window in the bone behind the ear (yellow circle). The photo below illustrates the incision behind the ear, as well as a small tube that is placed in the ear during the operation to monitor the patient’s hearing. The patient is asleep, but we are able to use this monitoring system to understand if we are putting too much tension on a nerve near the trigeminal nerve that supports hearing.

Here’s a view under the operating microscope. This is the view I have for much of the case that shows me the anatomy I need to see.
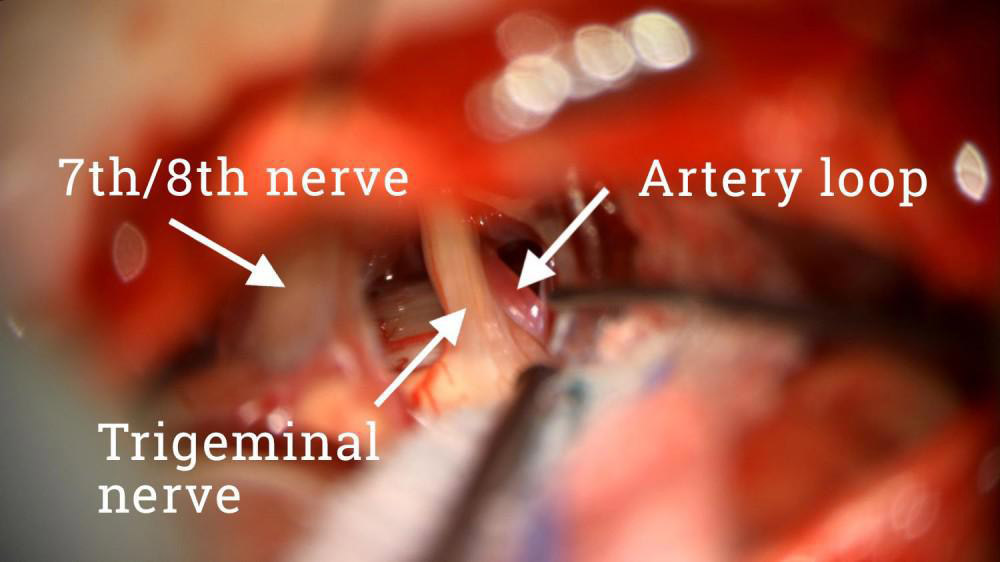
In the foreground are the 7th and 8th cranial nerves, which contribute to facial movements and hearing. Right next to the trigeminal nerve is the loop of the artery that we could see on the MRI. With each beat of the heart, that artery bangs into the side of the trigeminal nerve. My goal in an MVD surgery is to dissect the nerve and the artery apart.
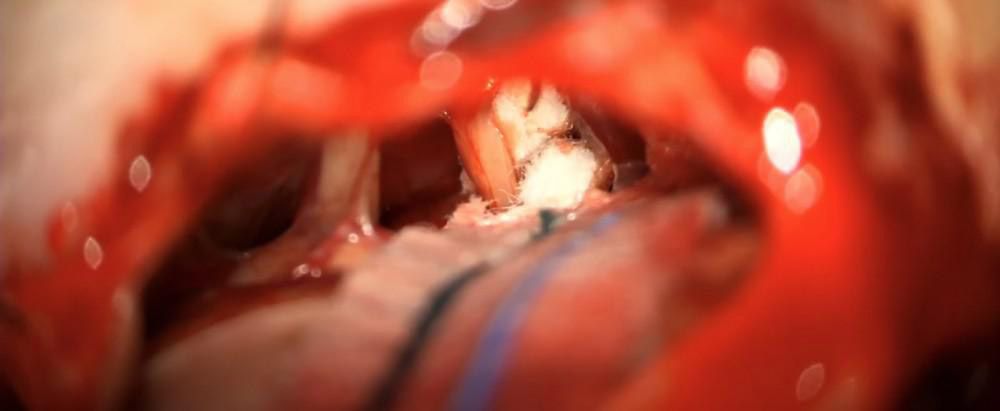
Because the artery has an elastic memory and falls back into place, I insert one or two pieces of teflon padding between the nerve and the artery to serve as a permanent shock absorber so that the artery doesn’t find its way back to the nerve. The nerve and the artery are now widely separated and the artery can no longer damage the trigeminal nerve.
What should you expect after MVD surgery? Facial pain improvement is often rapid. Most patients stay two nights in the hospital and one night in the intensive care unit. It’s very common to have a temporary period of nausea and some soreness around the area of the incision. I instruct patients not to reduce their trigeminal neuralgia medications right away; this is done later on as an outpatient.